Slow rollout of eating disorder services 'destroying lives'
Just four of the planned specialist eating disorder teams are operating, with recruitment issues cited by the HSE for the delay.

“IT IS CREATING a generation of people for whom their eating disorder is going to become so ingrained in their life and so difficult to let go, that more are going to have their lives destroyed or lose their lives.”
Like many impacted by eating disorders, Lisa Murphy is frustrated at the “slowness and delays” in the rollout of services across Ireland.
“We’ve seen what government can do when there’s an urgent situation and when there’s political will and I just don’t know why the urgency isn’t there.”
Murphy was responding to the latest figures released by the HSE in two parliamentary questions (PQs) which showed that just three of the 16 promised multidisciplinary teams for eating disorders (EDs) were operational as of December.
After publication of this article, a spokesperson for the HSE told Noteworthy that a fourth team began to accept referrals and complete assessments in the last quarter of 2022 “in line with their service development plans”. This article has been updated to reflect this.
Noteworthy requested an update from the HSE on this before publication as the PQs had stated this additional team would begin operation in Q1 2023 but we did not receive a clarification until a number of hours after the article was online.
The initial three teams were the only ones in place last year when Noteworthy investigated this issue. At the time, we found that only 55% of the staff for three additional teams promised for 2021 had been recruited.
- Noteworthy, the crowdfunded community-led investigative platform from The Journal, supports independent and impactful public interest journalism.
Minister for Mental Health Mary Butler told Noteworthy last February that “ring-fenced funding of €1.15 million for [2022], will enable the development of an additional five new specialist eating disorder teams, bringing the total number of teams to 11”.
Now, two HSE responses to parliamentary questions (PQs) by Sinn Féin spokesperson on mental health, TD Mark Ward, detail the progress on both the three teams promised in 2021 as well as three additional teams funded in 2022.

Updates on the nine teams – rather than 11 as Minister Butler had stated – show how issues with recruitment of positions have resulted in just one additional team being in place at the end of last year.
Premises are yet to be identified for a number of these teams also. The additional team in the Dublin North City and County area is currently being housed in a temporary building.
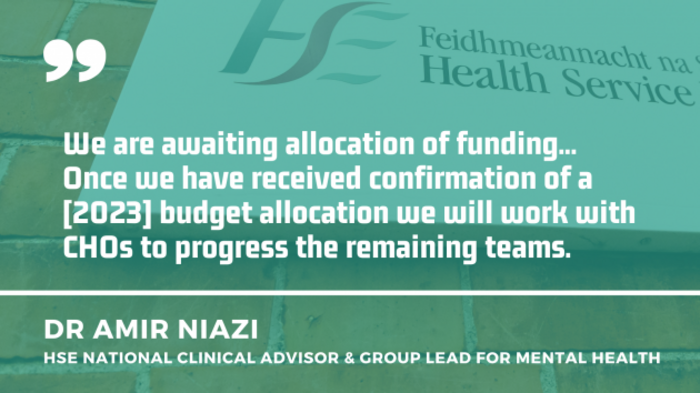
In the PQs, Dr Amir Niazi, national clinical advisor and group lead for mental health at the HSE wrote that €8m was “made available” for ED posts since 2016. This funding was spent on other mental health services in 2020 leading to planned ED developments being “temporarily paused”. Niazi continued:
“Recruitment of MDT teams requires 12-18 months duration in line with HSE recruitment procedures.”
Consultant posts not filled
The PQs detail recruitment issues including being unsuccessful in the hiring of an advertised consultant child and adolescent psychiatrist in Community Healthcare Organisation (CHO) Area 2, covering Galway, Mayo and Roscommon.
A successful candidate for the position of adult consultant psychiatrist in CHO 5, which covers a number of counties in the South East, did not accept the job. Both positions will now be re-advertised.
“The recruitment process has been impacted by the challenges in recruitment and retention experienced currently across the health service. Despite this all CHOs who have been allocated funding remain committed to recruiting staff and delivering community eating disorder teams,” the HSE’s Niazi wrote.
The HSE expects six of the nine funded teams “to be operational in 2023″, with the new team in Dublin North City and County now accepting referrals.
A spokesperson told Noteworthy that “a further seven teams are planned for in accordance with the Model of Care” but no dates were given as to when the full 16 teams would be in place. “All sites are committed to filling the posts and creating community eating disorder teams.”
Harriet Parson of Bodywhys, the Eating Disorders Association of Ireland told Noteworthy last year that this Model of Care was originally a five-year plan, to be implemented by 2023.
One of the key conclusions in the Model of Care is that “specialist ED teams have been associated with faster recovery, higher patient satisfaction, lower costs, lower rates of inpatient admission and better case identification”.
The PQ responses stated that it is recommended to deliver three eating disorder teams per year “to ensure sustainable phased recruitment and training”.
A spokesperson for CARED Ireland – a voluntary group of parents and carers of people with EDs – said that the delayed progress “is entirely unacceptable”.
“It appears that neither the HSE or the government is treating this illness with the seriousness and urgency it deserves, despite it having the highest mortality rate in mental health.
“Leadership within government and the HSE is now needed to ensure the ongoing delays and recruitment challenges are urgently addressed so that our loved ones get the services they are entitled to and can fully recover from this devastating illness.”
Budget 2023 not yet allocated
Sinn Féin’s Mark Ward said that “it is welcome” to see that ED teams “are progressing but Government should be focused on ensuring that service delivery is a priority”.
He added that funding from Budget 2023 “has not yet been allocated for eating disorders and needs to be allocated urgently”.
“With the high morbidity rates associated with eating disorders and the amount of people presenting for treatment with eating disorders having increased over the last few years, as reported by Bodywhys, it is important that Government resources the HSE to meet its targets on time.”
Rates of eating disorders have been increasing for the past number of years. A spokesperson for the HSE told Noteworthy that “referral rates remain well above the predicted demand prior to the pandemic and significantly higher than referral rates in 2019 (2.5 fold increase)”.
The spokesperson said that “Budget 2023 sees an additional €72.8 million of funding for mental health services” bringing its total investment “to over €1.2 billion”.
In his PQ responses, the HSE’s Niazi stated that “the fourth phase of teams have been identified and relevant CHOs have submitted business cases including advance planning to support recruitment and identification of team premises”.
Lisa Murphy is calling on the government to fund treatment in the private sector, especially for people who do not fall inside the catchment area of the teams currently in operation.
“Early intervention is key, particularly for eating disorders. The longer [EDs] go on, the more they become part of your identity. They become your whole world.
“We’re going to have more people on waiting lists. People not able to access care because of where they live.”
In order to get access to treatment, Murphy resorted to crowdfunding for private inpatient treatment in 2021 when she was unable to secure HSE funding for treatment for bulimia. She raised almost €65,000 within a few days.
She told Noteworthy that a number of people have contacted her in recent months also exploring that option.
She has also been in touch with families spending thousands to fund day or inpatient treatment. Many people who spoke to us as part of our investigation last year also told us of the thousands they spent due to lack of public care.
“If you get the right time, right team, right place, [treatment] does work.”
Updated at 9.30pm on 11 January to include HSE response on the additional specialist team.
If you need to speak to someone, contact:
- Bodywhys: 01 210 7906 (opening hours) or email alex@bodywhys.ie (eating disorders)
- HSE Eating Disorder Self Care App (information on eating disorders)
- CARED Ireland: email caredireland@gmail.com (group of parents and carers of people with eating disorders)
- Samaritans: 116 123 or email jo@samaritans.ie
- Aware: 1800 80 48 48 or email supportmail@aware.ie (depression, anxiety)
- Pieta House: 1800 247 247 or email mary@pieta.ie (suicide, self-harm)
- Childline: 1800 66 66 66 (for under 18s)
- Teenline: 1800 833 634 (for ages 13 to 18)
—

This is a follow-up to our award-winning investigation which found that the health system is failing people with eating disorders

By Maria Delaney of Noteworthy
Noteworthy is the crowdfunded community-driven investigative platform from The Journal that supports independent and impactful public interest journalism.
Please support our work by submitting an idea, helping to fund a project or setting up a monthly contribution to our investigative fund HERE>>






